What is FPIES?:


FPIES, more formally known as Food Protein-Induced Enterocolitis Syndrome, is a disorder that causes an allergic reaction to food in the gastrointestinal system. FPIES is one of the more prevalent non-immunoglobulin E (IgE) disorders. The most common symptoms of FPIES are intense vomiting and diarrhea.
However, the most distinguishing symptom of FPIES is that the reaction to the consumption of a trigger food is delayed by two hours or more. The other possible symptoms include lethargy and abdominal swelling. Though FPIES is most common in children under the age of three (as it typically resolves itself anywhere past that age), it is still very possible for it to persist throughout childhood and potentially into adulthood. The most common trigger foods in children are dairy, soy, and rice. Alternatively, the most common trigger food in adults is shellfish. In some severe cases of FPIES in infants, acute dehydration, hypovolemic shock, and hypotension are also possible and incredibly dangerous. FPIES can cause young children to not grow or gain weight at the rate they should.
Logan was 11 weeks old when she was switched to dairy-based formula, which she had handled well on three occasions. She was given a bottle and set down for a nap before she woke up two hours later, vomiting profusely until it was green bile. Her parents, Kerry and Tim, rushed her to the emergency room near their home. They brought the formula with them, thinking it could be related to her episode. The doctors told them that because Logan hadn’t reacted to the formula previously, the formula probably wasn’t the cause of her episode. After spending a night in the ER being monitored, Logan was discharged. Then, two weeks later, she drank the same formula, her parents having been assured the formula was safe but she had a similar severe vomiting episode and was brought to the hospital again. It was during this visit that the doctor speculated Logan might have FPIES. After some questions and googling, Kerry and Tim learned how it was normal for a child with FPIES to feel okay after ingesting their trigger food the first couple of times.
What are the Causes of FPIES?:
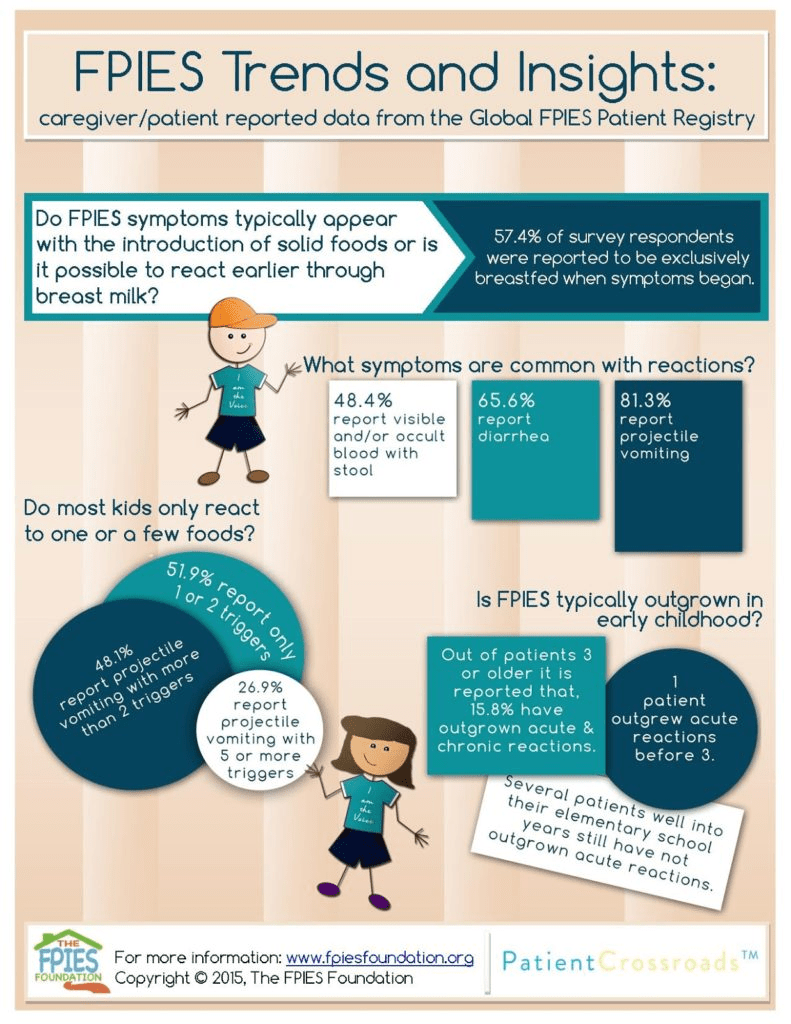
The exact cause of FPIES is unknown (which is why we need to raise more awareness so more research can be done!), and it is not IgE-mediated like other allergies, which makes it harder to identify the root cause.
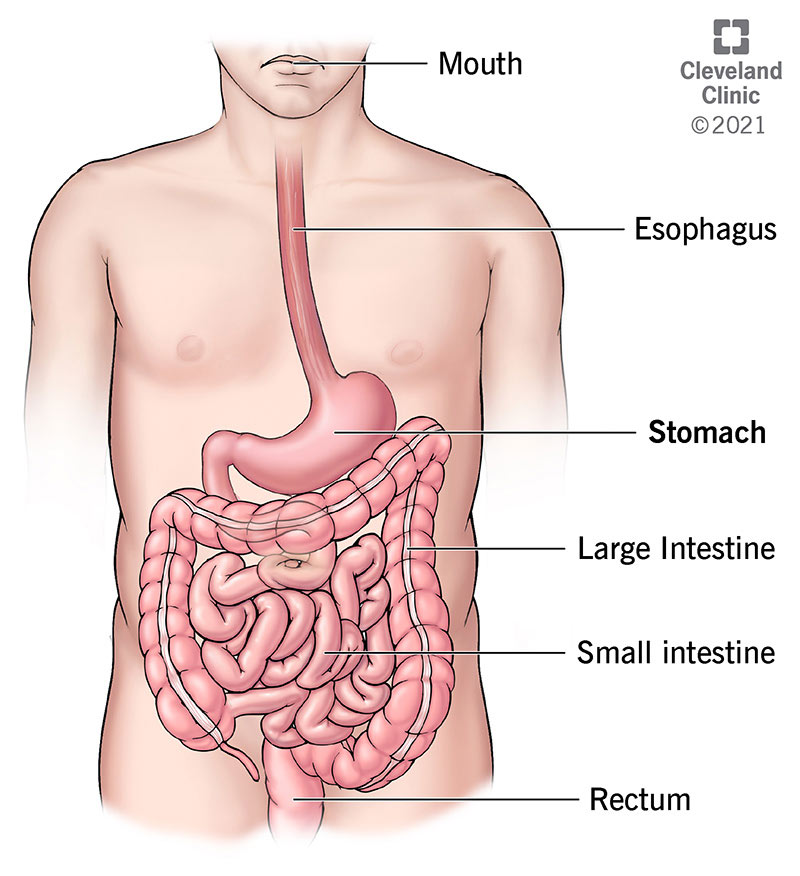
However, the most current studies have investigated the possibility of FPIES being caused by an irregular immune response to the specific proteins found in a particular food. It’s speculated that the trigger food inflames the large and small intestines, presumably meant to allow fluids and other substances to pass through the intestinal wall. Cell-mediated immune responses are responsible for fighting off viruses, and they do not involve antibodies like IgE. However, the humoral immune response fights infection caused by other viruses and bacteria.
Additionally, this response does include antibodies. Some research suggests that T cells (the cells involved in the cell-mediated immune response) are essential to the development of inflammation in the intestinal tract in the case of FPIES, but this has yet to be fully confirmed. It is also likely that the cell-mediated response contributes to the inflammation. One primary function of T cells is the production of cytokines, which are specific proteins secreted from immune system cells to either stimulate or inhibit the function of other cells. Some cytokines help to regulate the body’s inflammatory response to disease. These proinflammatory cytokines (such as tumor necrosis factor-alpha and thymus and activation-regulated chemokine (TARC)) could be key factors in the development of FPIES. It is not yet confirmed whether or not FPIES is caused by genetic or environmental stimuli.
How is FPIES Diagnosed?:


FPIES is diagnosed based on the identification of the distinguishing symptoms through clinical evaluation. The lack of symptoms commonly associated with regular IgE-based allergies can also be indicative of FPIES. FPIES is often misdiagnosed due to its potential similarity to other diseases and the lack of skin and blood tests to confirm. This could also lead to a delay in diagnosis. In 2017, guidelines were officially published to aid in diagnosing FPIES. These guidelines distinguish between acute and chronic FPIES. According to the guidelines, chronic FPIES includes the recovery from symptoms soon after eliminating the trigger food from one’s diet.
Kerry and Tim visited an “FPIES Clinic” and met with their gastroenterologist (GI). Logan was then tested for any genetic conditions that could be causing her reaction. However, all of those tests came back negative. After that, since Logan was tolerating breastmilk well and gaining weight steadily, the GI doctor discharged her as there was really nothing else they could do for her at that time.
As previously mentioned, there is no skin or blood test to diagnose FPIES, so Logan was assessed based on her symptoms. When her symptoms were analyzed, Logan was officially diagnosed with FPIES by her allergy doctor. Logan’s family also met with a registered dietitian who helped them learn how to introduce solid food to her. They were informed they would have to feed her using “food trials.” They began these trials when she was 7 months old, giving her small amounts of food and then increasing the amount each day, one week at a time. Once it was noted that she was tolerating the food without reacting, her parents would try another food. They eventually discovered that Logan had no other trigger foods besides dairy.
What is the Treatment for FPIES?:

Removing the trigger food(s) typically leads to the disappearance of symptoms in affected people. Children tend to grow out of FPIES sometime between two and four years of age. Infants are recommended to breastfeed exclusively, but as they grow older, they need supplemental foods to have enough calories for the day. This could be resolved by using an elemental amino acid formula. The most severe episodes of FPIES require medical intervention. This will generally involve the use of intravenous fluids. Some physicians use anti-inflammatory drugs like corticosteroids to help affected individuals during an episode. For those acute FPIES reactions, it’s been suggested to use ondansetron intravenous for acute symptoms of vomiting. Many children with FPIES may develop food aversion, poor weight gain, and nutritional deficiencies, as previously mentioned. This makes dietary management crucial. This means avoiding the food that triggers the symptoms, adding supplemental foods to encourage regular growth, and providing families with individualized feeding plans. One particular study investigated an alternative treatment option called oral desensitization, also known as oral immunotherapy treatment (OIT), and is utilized in managing IgE-mediated food allergies to desensitize the body to the allergen. This allows the patient to eat the food without risk of an FPIES episode.
For Kerry and Tim, helping Logan avoid her trigger foods requires enormous vigilance. However, since Logan’s trigger food is dairy, it is slightly less burdensome for her family to determine if her food has any dairy products in it, as dairy-based ingredients are clearly labeled on most food products.
Since her diagnosis five years ago, Logan has been given various forms of dairy, including baked dairy and cooked dairy. This gradual reintroduction is solely for dairy products where the milk protein has been significantly altered by cooking or processing. Thus far, Logan has been tolerating these forms of milk just fine! Although she still cannot tolerate other forms, like a glass of milk or ice cream, she can tolerate a lot more than when she was initially diagnosed. Logan has also become her own advocate as she even asks her parents, “Does this have milk in it?” before she eats something.
Life with FPIES:


FPIES became Kerry and Tim’s entire focus to ensure Logan’s safety and happiness. Nearly five years later, Logan’s parents feel incredibly confident navigating their daughter’s diagnosis. At first, for Kerry and Tim, feeding Logan was terrifying, and they constantly felt on edge, worried that she would have another reaction. They had to allocate additional money for buying expensive allergy-friendly food.
Kerry and Tim struggled with the idea of Logan being “excluded” at birthday and holiday parties. As everyone can appreciate, food is a very social aspect of life, and Logan was not always able to be included. Halloween and other holidays revolving around food were stressful for her parents. Logan couldn’t always participate in the same way as other kids but Kerry and Tim always make certain Logan has a special lunch box of foods and treats she can have.
Logan’s parents had to watch her like a hawk when she was younger so that she never tried to reach for food or eat something that was not safe. She was taught to only eat food given to her by her family. Eyes had to be glued to her at all times if she went to someone’s house. Once Logan turned 3 years old, she began to understand that she couldn’t touch food or try to eat it unless it was her “special food.” It became tricky for Kerry and Tim to take Logan on vacation or travel too far from their house as they needed a lot of space to prepare Logan’s food. They opted to stay home until they figured out a system to handle Logan’s food safely. Even sending her to school made Kerry and Tim extremely nervous, but her teachers have been very good at keeping her safe. Seeing other kids with allergies at her school helped show Logan that she wasn’t alone. Fortunately, now, at five years old, Logan is nearly FPIES free!
There is still so much more to be learned about FPIES, and unavoidably, more children will be diagnosed. To see how you can raise awareness or contribute to FPIES research, please visit the FPIES Foundation!
References:
Alyea, G., Spergel, J. M., & Starr, S. E. (2024, July 15). Food Protein-Induced Enterocolitis Syndrome – Symptoms, Causes, Treatment: NORD. National Organization for Rare Disorders. https://rarediseases.org/rare-diseases/food-protein-induced-enterocolitis-syndrome/
Special thank you to Kerry and Tim for taking the time to talk with me! (And thank you, Logan!)
Let’s keep spreading awareness! – Lily
Leave a comment