What is FOP?:
Episodic flare-ups (inflammatory swelling of soft tissues) in FOP typically start in early childhood and continue to worsen over time. The majority of FOP cases arise from a spontaneous mutation in the ACVR1 gene, which is part of the bone morphogenetic protein (BMP) signaling pathway. This pathway plays a crucial role in both the development of the skeleton during embryonic stages and the repair of the skeleton after birth.
Symptoms:
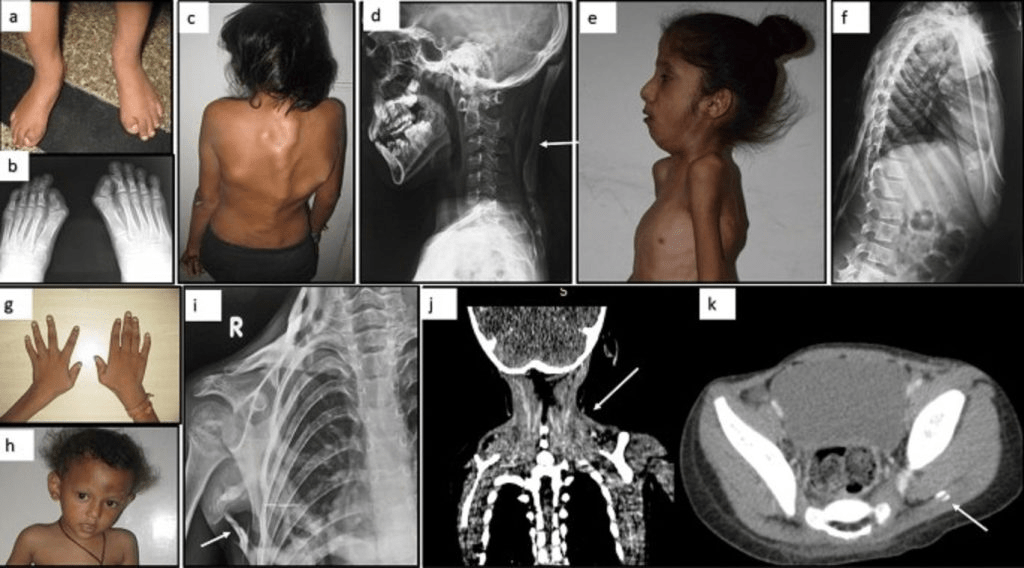
FOP is characterized by congenital malformations, most notably of the great toes and, in about 50% of cases, the thumbs. These skeletal abnormalities are present at birth and are the earliest signs of the condition. The common malformation includes a shortened great toe with an abnormal distal first metatarsal and missing or malformed phalanx. Other toe and finger issues include hallux valgus, microdactyly, and clinodactyly. Additional congenital features can involve osteochondromas in the tibia, cervical vertebrae malformations, and an abnormally short femur.
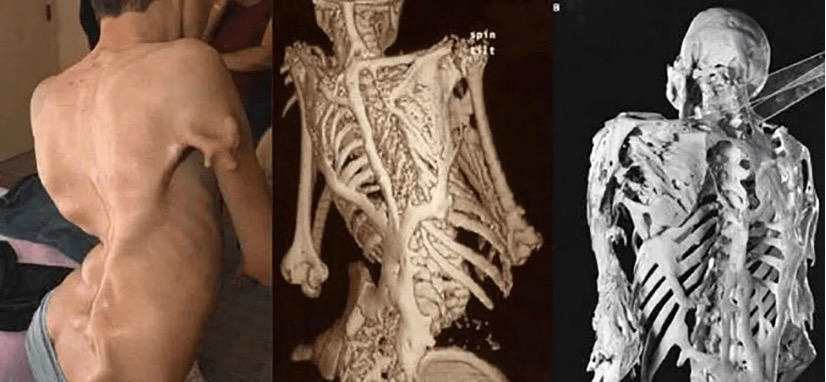
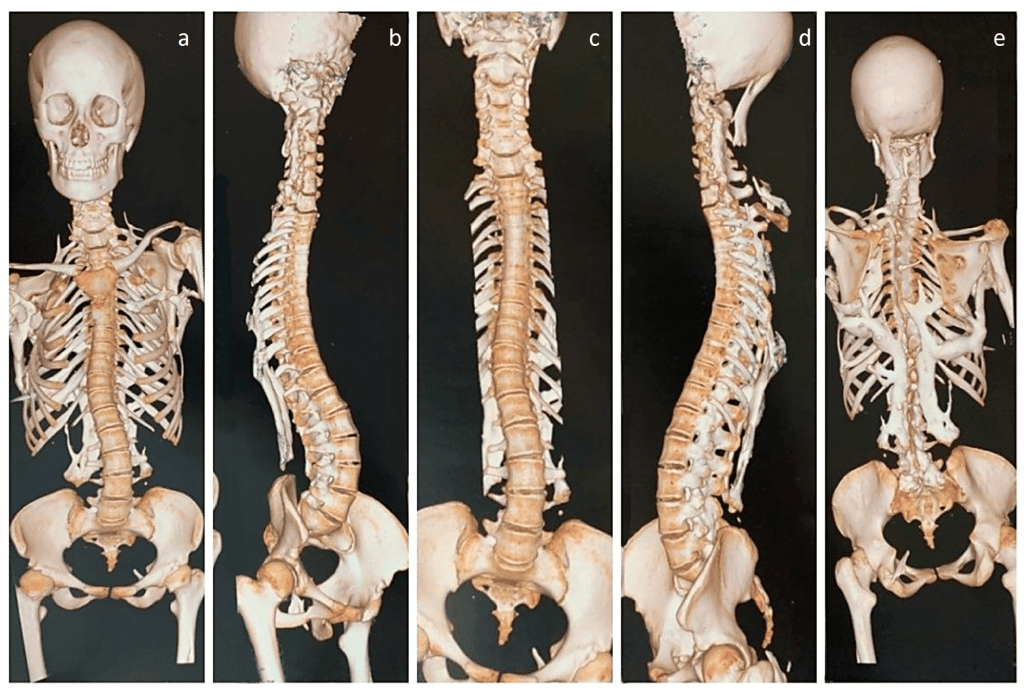
Progressive bone growth in connective tissues (heterotopic ossification) usually begins in early childhood, often triggered by injury or illness. This leads to tender, swollen areas, typically in the back, neck, and shoulders, which mature into bone through a cartilage-to-bone process. Over time, bone forms in tendons, ligaments, muscles, and connective tissues, causing pain, stiffness, and potential low-grade fever. The bone growth progresses, affecting various body areas, including the hips, ankles, and jaw, eventually leading to stiffness and limited mobility in joints.
Chronic swelling is common and may result from abnormal bone growth pressing on lymphatic vessels or lack of muscle movement, causing fluid buildup. As the disease advances, joint stiffness, spinal deformities (scoliosis and kyphosis), and restricted movement occur. Severe cases lead to full immobilization, difficulty with balance and walking, and possible nerve compression, resulting in pain and dysfunction. FOP can also lead to respiratory infections, heart failure, hearing loss, and, in some cases, hair loss or mild cognitive delay. The progression of FOP can vary significantly between individuals, even among identical twins.
Causes:
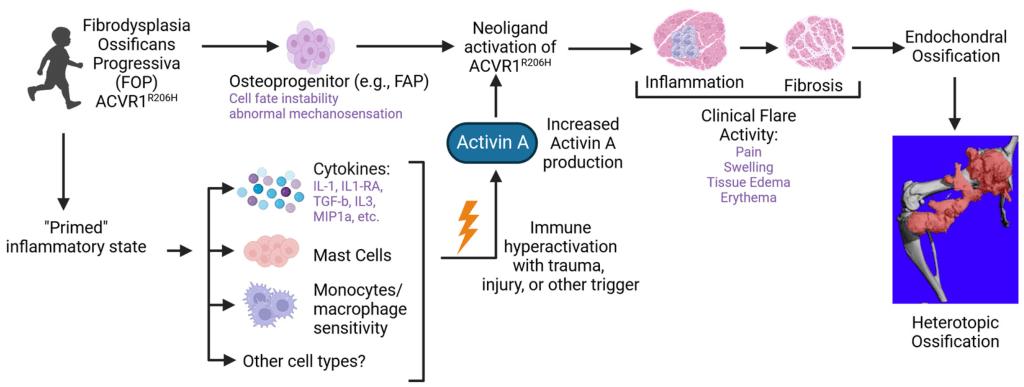
Most cases of FOP occur sporadically, affecting a single individual in a family. However, when FOP follows a familial pattern, it is inherited in an autosomal dominant manner, meaning that only one copy of the mutated gene is needed to cause the disorder. This gene variant can either be inherited from a parent or result from a new mutation in the affected individual. If inherited, each child of an affected parent has a 50% chance of inheriting the gene, with the risk being the same for both males and females.
In 2006, researchers identified the genetic cause of FOP. They discovered that a mutation in the ACVR1 gene, part of the bone morphogenetic protein (BMP) signaling pathway, is responsible for the disorder. BMPs are essential for skeletal formation during embryonic development and for post-birth bone repair. The ACVR1 gene encodes a receptor (activin receptor type IA) that is involved in the signaling pathway. A specific mutation in the ACVR1 gene, where an amino acid called arginine at position 206 is replaced by histidine, causes abnormal activation of the ACVR1 receptor, triggering the disease.
Diagnosis and Treatment:
FOP is often misdiagnosed, but it can be identified by checking for the characteristic short great toes. Diagnosis is confirmed through a thorough clinical evaluation, physical findings, and genetic testing for mutations in the ACVR1 gene. Biopsies should be avoided, as they can trigger rapid bone formation in the affected areas. Additionally, intramuscular injections, local anesthetic use, jaw stretching for dental procedures, and trauma should be avoided, as these can provoke flare-ups. Viral infections, like the flu, can also trigger flare-ups.
In 2023, the FDA approved palovarotene, a medication that helps reduce abnormal bone growth in individuals with FOP aged 8 years and older (10 for males). Preventative antibiotics may be necessary for those at higher risk of respiratory infections due to limited mobility.
Pain and swelling from flare-ups can be managed with corticosteroids and non-steroidal anti-inflammatory drugs. Occupational therapy, along with special shoes, braces, and other mobility aids, can help individuals with FOP maintain daily activities. A team approach, including social, educational, and medical services, is recommended for infants diagnosed with FOP. Genetic counseling is also advised for affected individuals and their families. Other treatments focus on symptom management and support.
How You Can Make an Impact:
Without proper research, funding, and support for continued studies and clinical trials to determine possible cures, legitimate medicines for the disease, or preventative treatment, many more people will go on to develop Fibrodysplasia Ossificans Progressiva. If you can, please donate here! If you are unable to donate, consider volunteering your time by raising awareness for this rare disease. If you’re interested in learning more about FOP, donation opportunities, or the progress being made on potential treatments, visit the International Fibrodysplasia Ossificans Progressiva Association! The International Fibrodysplasia Ossificans Progressiva Association strives to “fund research to find a cure for FOP while supporting, connecting and advocating for individuals with FOP and their families, and raising awareness worldwide.”
References:
Kaplan, F., & Shore, E. (2024, June 26). Fibrodysplasia Ossificans Progressiva – Symptoms, Causes, Treatment | NORD. NORD (National Organization for Rare Disorders); NORD. https://rarediseases.org/rare-diseases/fibrodysplasia-ossificans-progressiva/
Let’s keep spreading awareness! – Lily
Leave a comment