What is Oculocutaneous Albinism:
Oculocutaneous albinism (OCA) refers to a group of rare genetic disorders that lead to little or no melanin production in the skin, hair, and eyes. It results from mutations in specific genes responsible for melanin creation in melanocytes. The lack of melanin causes light skin that is highly prone to sun damage, including skin cancer, and affects eye development, leading to vision issues such as involuntary eye movements (nystagmus), crossed eyes (strabismus), and light sensitivity (photophobia). Additional eye abnormalities include underdevelopment of the retina (foveal hypoplasia) and misrouting of the optic nerves. While all individuals with OCA share these vision problems, the degree of pigment in the skin, hair, and eyes varies depending on the gene mutation and OCA type.
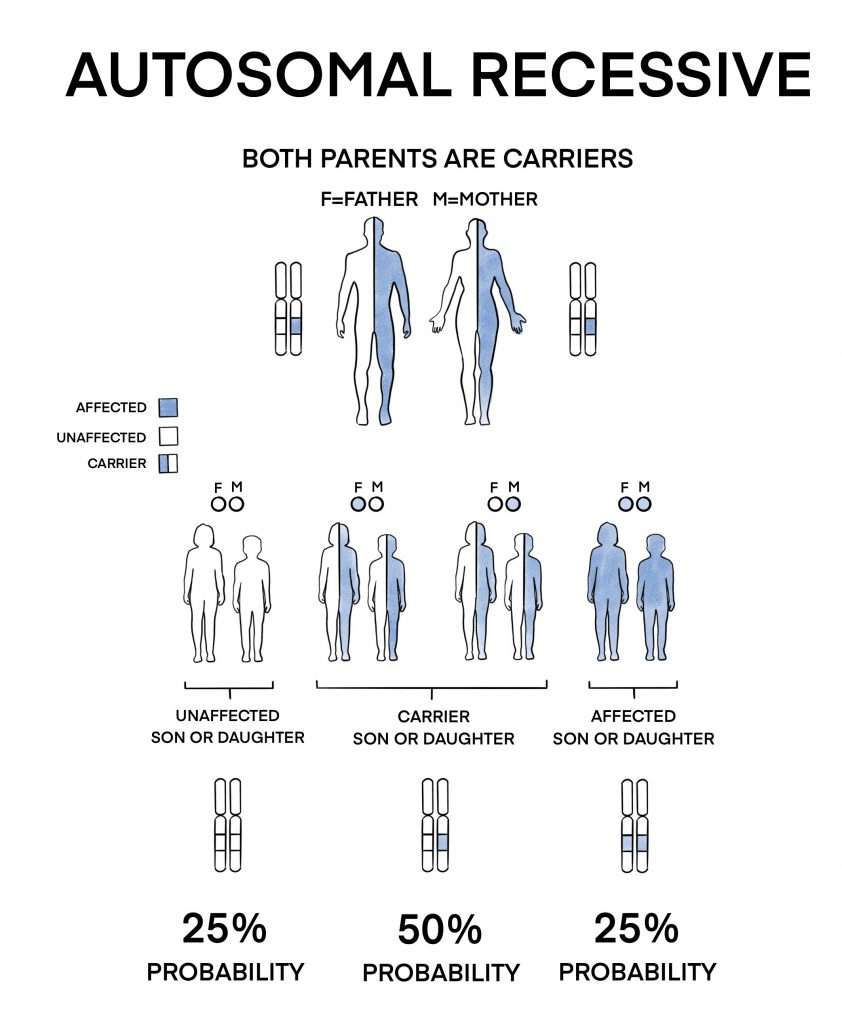
There are seven known types of OCA (OCA1 through OCA7), each linked to mutations in a different gene. The condition is inherited in an autosomal recessive pattern.
Symptoms:
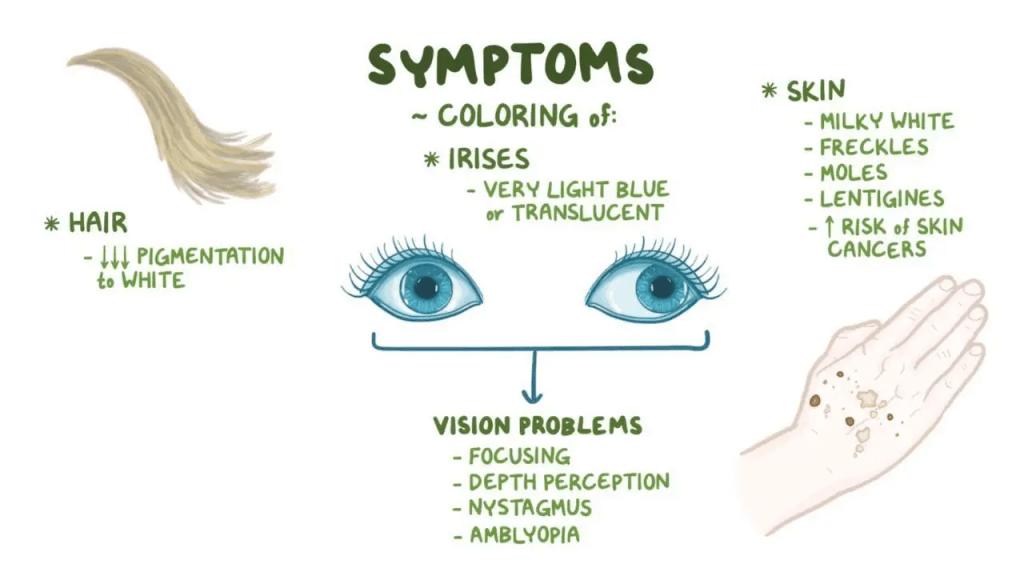
Oculocutaneous albinism (OCA) is associated with a range of vision problems caused by reduced or absent melanin pigment in the eyes. Common issues include involuntary eye movements (nystagmus), reduced pigmentation in the iris (iris transillumination) and retina, underdevelopment of the macula (macular hypoplasia), and abnormal visual pathways between the retina and brain, which can lead to misalignment of the eyes (strabismus) and poor depth perception. These abnormalities result in reduced visual acuity, typically ranging from 20/60 to 20/400, with better vision generally seen in individuals who have more eye pigment.
Oculocutaneous albinism type 2 (OCA2) presents the same vision problems as OCA1, but affected individuals tend to have a broader range of skin and hair pigmentation, influenced by their genetic background and the specific mutation involved. Unlike in OCA1, the hair in OCA2 is usually not completely white, and the skin often contains some pigment, though it remains lighter than that of unaffected family members. People with darker skin tones, such as Africans and African-Americans, show noticeable pigment loss, while those with naturally lighter skin may appear close to normal but still lack the ability to tan. A unique feature of OCA2 is the development of pigmented spots (nevi and lentigines) with sun exposure, which is not seen in other OCA types. A subtype called brown OCA, found only in individuals of African descent, features darker hair and skin. OCA2 results from mutations in the OCA2 gene, previously known as the P gene.
Oculocutaneous albinism type 3 (OCA3), initially described in African populations and also known as rufous albinism, is characterized by reddish to red-brown skin, ginger or reddish hair, and hazel or brown eyes. It has since been identified in various other groups, including individuals of Asian, Indian, and Northern European descent. Among people of Asian heritage, affected individuals may have blond hair, light brown eyebrows, and skin lighter than their parents, with both hair and skin pigmentation increasing with age. Vision problems in OCA3 are generally less severe than in OCA1 and OCA2, and symptoms like nystagmus and photophobia may be absent. OCA3 is caused by mutations in the TYRP1 gene, which encodes tyrosinase-related protein 1.
Oculocutaneous albinism type 4 (OCA4) resembles OCA2 in terms of physical features. Hair color ranges from yellow to brown, and visual acuity can vary widely, from 20/30 to 20/400, although it typically stabilizes between 20/100 and 20/200 after childhood. OCA4 was first reported in an individual of Turkish origin and is more frequently found in Japanese, Korean, and German populations. This type of OCA is linked to mutations in the SLC45A2 gene, previously known as MATP, which encodes a membrane-associated transport protein. While all forms of OCA share core characteristics related to pigmentation and vision, the severity of symptoms and the extent of pigmentation vary based on the type and genetic background.
Causes:
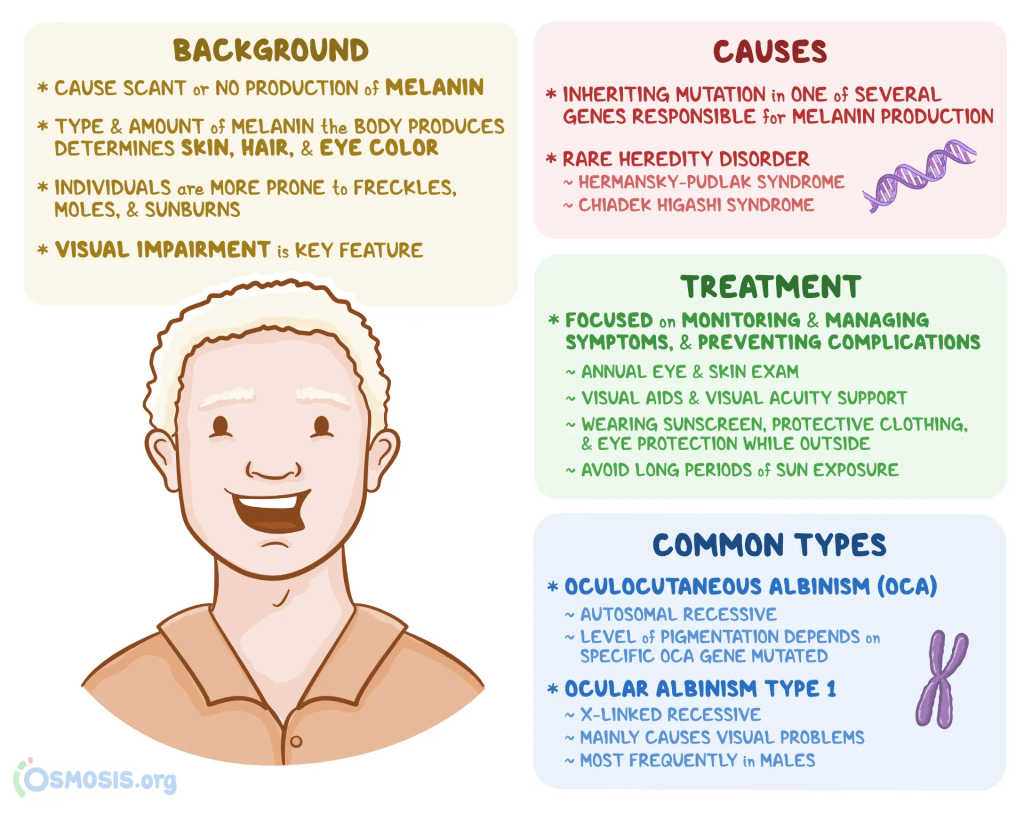
Melanin is the primary pigment responsible for the color of the skin, hair, and eyes. It exists in two forms: brown-black eumelanin and yellow-red pheomelanin, with all melanin being a mixture of these two types. Melanin is produced by specialized cells called melanocytes. When mutations occur in genes that produce the proteins needed for melanocytes to make melanin, it leads to a reduction or complete lack of pigment, resulting in a condition known as oculocutaneous albinism (OCA). OCA is inherited in an autosomal recessive pattern, meaning a person must inherit two faulty copies of the gene (one from each parent) to be affected. Carriers, who have one normal and one mutated gene, typically do not show symptoms. When both parents are carriers, there is a 25% chance with each pregnancy that the child will have OCA, a 50% chance the child will be a carrier, and a 25% chance the child will inherit two normal genes. These risks are the same for both boys and girls.
Seven genes have been linked to the different types of OCA, and all are crucial to melanin production within melanocytes, which are located in the skin, hair follicles, iris, and retina. In the skin and hair, melanocytes transfer melanin to keratinocytes (the cells that give skin and hair their color). In the eyes, pigment is produced in both the iris and the retinal pigment epithelium. Different types of oculocutaneous albinism have many different causes, though.
Diagnosis:

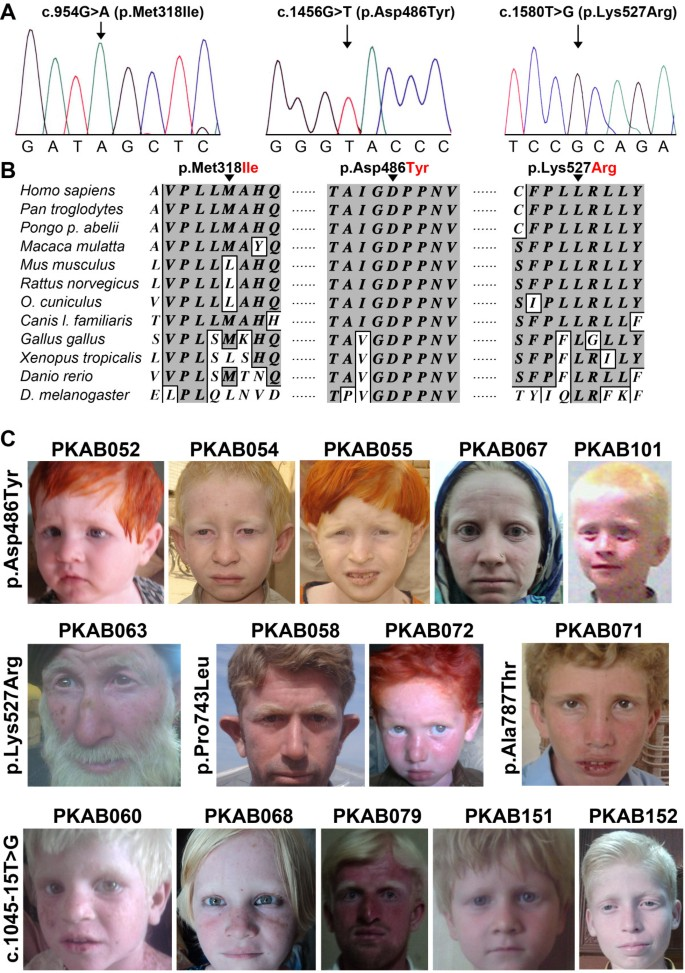
While physical traits can offer clues about the type of albinism, accurate diagnosis of the specific type of Oculocutaneous Albinism (OCA) requires DNA sequencing of the seven associated genes. For individuals of African descent, it is especially important to test for a specific 2.7 kb exon deletion in the OCA2 gene, which is commonly linked to OCA in this population.
Treatment:
People diagnosed with Oculocutaneous Albinism (OCA) should see an ophthalmologist at the time of diagnosis to assess the condition’s severity and continue with yearly eye exams. Vision may improve over time, and corrective lenses like glasses or contacts can help. Because those with OCA are often sensitive to light, wearing dark sunglasses or a wide-brimmed hat can ease discomfort. It’s also important to evaluate how much pigment is present in the skin. To prevent sunburn, skin damage, and skin cancer, individuals should protect their skin using sunscreen and protective clothing. Skin care advice will vary based on the person’s level of pigmentation.
How You Can Make an Impact:
Without proper research, funding, and support for continued studies and clinical trials to determine possible cures, legitimate medicines for the disease, or preventative treatment, many more people will go on to develop Oculocutaneous Albinism. If you can, please donate here! If you are unable to donate, consider volunteering your time by raising awareness for this rare disorder. If you’re interested in learning more about Oculocutaneous Albinism, donation opportunities, or the progress being made on potential treatments, visit the National Organization for Albinism and Hypopigmentation! NOAH strives “to act as a conduit for accurate and authoritative information about all aspects of living with albinism and to provide a place where people with albinism and their families in the U.S. and Canada can find acceptance, support and fellowship.”
References:
Oetting, W. (2015, August 18). Oculocutaneous Albinism – Symptoms, Causes, Treatment | NORD. NORD (National Organization for Rare Disorders); NORD. https://rarediseases.org/rare-diseases/oculocutaneous-albinism/
Leave a comment