What is Pediatric Crohn’s Disease?:
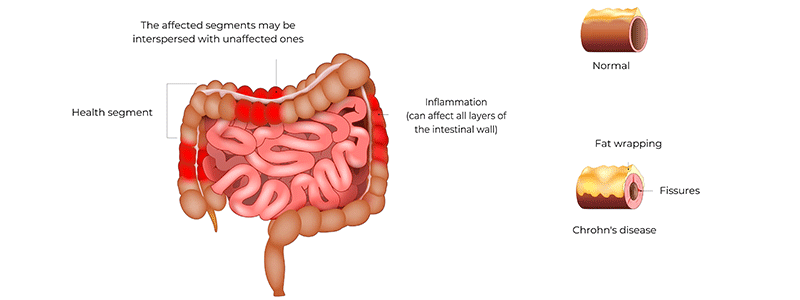
Pediatric Crohn’s disease is a rare type of inflammatory bowel disease that causes long-term inflammation in the lining of the digestive tract. The gastrointestinal tract includes the organs that connect from the mouth to the anus, such as the esophagus, stomach, small intestine, large intestine, and anus. The esophagus carries food from the throat to the stomach, while the small intestine continues digestion and absorbs most nutrients and water. When the small intestine is damaged or removed, the body may not absorb enough vitamins, minerals, and other nutrients. The large intestine connects the small intestine to the anus and is responsible for absorbing water and minerals as well as forming and storing solid waste before it leaves the body through the rectum and anus. Pediatric Crohn’s disease can affect any part of this system, but it most commonly involves the ileum, which is the last part of the small intestine, and the large intestine.
Children with Crohn’s disease often experience diarrhea, abdominal pain, fever, and weight loss. Growth delays and difficulty gaining weight may also be early signs, which can sometimes lead to a delay in diagnosis. The disease tends to come and go, with periods of active symptoms followed by times of improvement. Although Crohn’s disease is more frequently diagnosed in adults, about one in four cases occur in children and teenagers. Young patients are less likely than adults to have disease limited only to the small intestine. The exact cause of pediatric Crohn’s disease is not known, but it is believed to result from a combination of genetic predisposition, immune system problems, and environmental factors.
Symptoms:
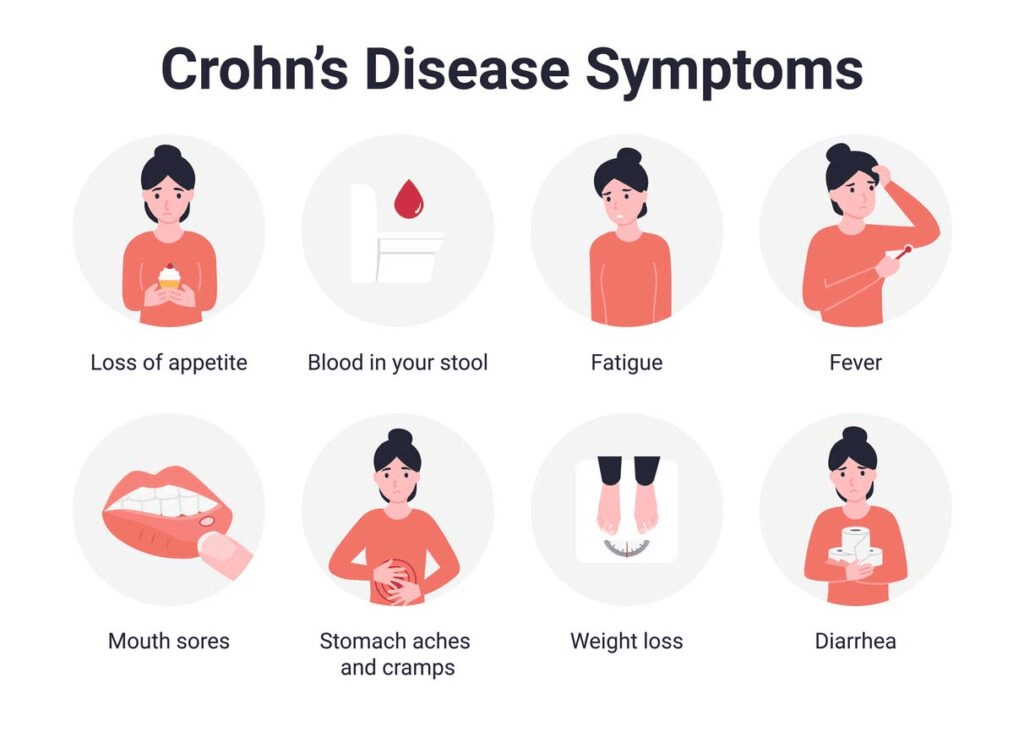
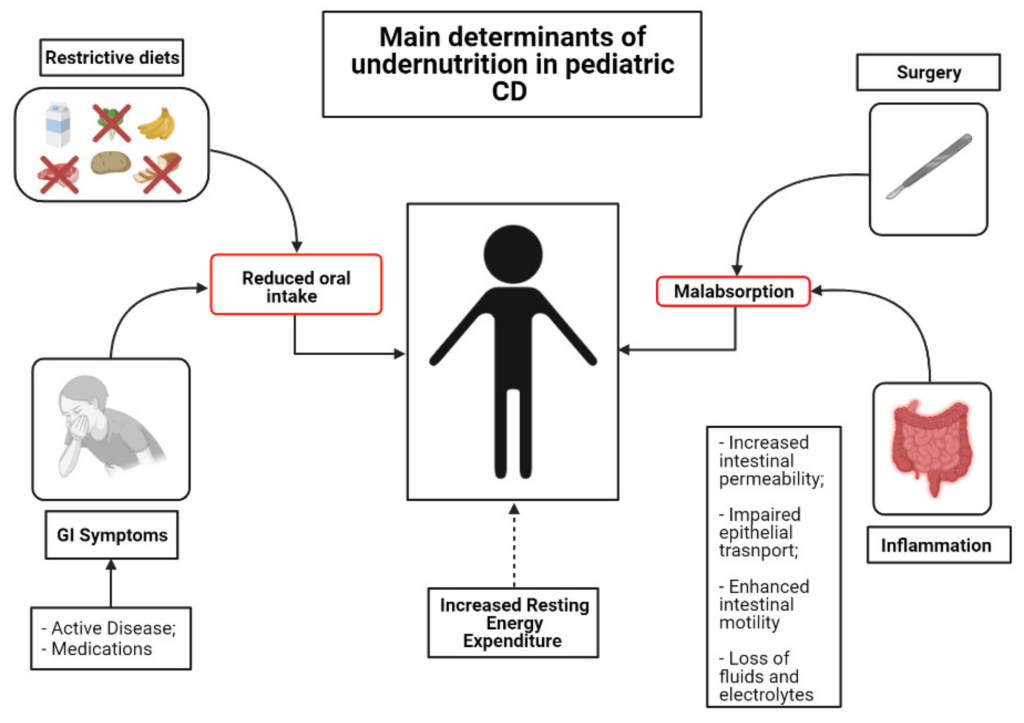
The signs and symptoms of pediatric Crohn’s disease can differ from one child to another and may appear suddenly or develop gradually over time. They can be triggered by factors such as illness, stress, or injury, although sometimes they occur without a clear cause. Common symptoms include cramping, abdominal pain, and frequent watery diarrhea, which may occasionally contain blood. Many children feel an urgent need to use the bathroom and may experience fatigue, fever, nausea, and loss of appetite. Poor appetite can lead to difficulties with weight gain and normal growth, and some children may develop malnutrition or have trouble absorbing nutrients from food. As a result, growth delays and delayed puberty can occur.
Some children experience bleeding in the digestive tract that is not always visible, which can lead to anemia. Anemia is a condition marked by low levels of red blood cells that carry oxygen throughout the body, and it can cause tiredness, pale skin, and lightheadedness. About one-third of children with Crohn’s disease develop perianal disease, which affects the area around the anus and can make bowel movements painful. This may cause tears, abscesses, or fistulas, which are abnormal connections between the skin and the inside of the anus. Some children may also develop small skin tags near the anus.
Over time, inflammation can cause scar tissue to form in the intestines, leading to narrowing known as a stricture. This can block the normal passage of food and result in bowel obstruction, which may cause cramping, vomiting, and constipation.
In addition to digestive problems, some children develop extraintestinal symptoms that affect other parts of the body. About 40% may have mouth lesions such as sores on the gums or lining of the mouth, canker sores, or swelling. In rare cases, children may have mouth and anal lesions with only mild intestinal disease. Other possible symptoms include painful red bumps on the skin known as erythema nodosum, eye inflammation that causes burning or itching, and joint pain or arthritis.
Causes:
The exact cause of pediatric Crohn’s disease is not fully known, but it is believed to result from a combination of genetic, immune system, and environmental factors. This means that several influences must act together for the disease to develop. One major factor appears to be an abnormal immune system response. Normally, the immune system protects the body from harmful invaders such as bacteria and viruses. In children with Crohn’s disease, however, the immune system becomes overactive after being triggered, often by an infection, and does not turn off as it should. Instead, it mistakenly attacks the tissues of the digestive tract, especially the small and large intestines. This ongoing immune activity causes chronic inflammation and irritation, which lead to the symptoms of the disease. Scientists are still trying to understand why the immune system behaves this way and why it targets the digestive system.
Genetics also play an important role. Children with a family history of Crohn’s disease are more likely to develop the condition than those without one, and about 15% of affected children have a relative with the disease. Having certain genes may make someone more likely to develop Crohn’s, but other environmental or immune factors are usually needed to trigger it. Variations in several genes, including NOD2, ATG16L1, IL23R, and IRGM, have been linked to pediatric Crohn’s disease. These genes help regulate the immune system, and when they are altered, the immune response may not work properly. Scientists have identified more than 200 genes associated with Crohn’s disease and ulcerative colitis, and they are studying how specific genetic changes may relate to particular symptoms or disease patterns. Some severe cases of Crohn’s disease that appear at birth or shortly after are linked to changes in genes involved in the interleukin 10 signaling pathway. Interleukin 10 normally helps reduce inflammation, and when these genes are altered, inflammation can become uncontrolled.
Environmental influences may also contribute to the development of pediatric Crohn’s disease. Infections caused by bacteria or viruses might directly harm the intestines or activate the immune system in a way that leads to self-damage. Other possible risk factors include frequent use of antibiotics, eating a Western-style diet high in processed foods, and exposure to cigarette smoke. The community of bacteria living in the intestines, known as the gut microbiota, also appears to play an important role. Some gut bacteria are beneficial and help regulate the immune system, while others may promote inflammation. When the balance of these bacteria is disturbed, it may increase the risk of Crohn’s disease, although researchers do not yet fully understand how or why these changes occur.
Diagnosis:
Diagnosing pediatric Crohn’s disease involves identifying characteristic symptoms, reviewing the child’s medical and family history, performing a thorough physical examination, and conducting several specialized tests. Doctors may suspect the disease in children or teenagers who experience long-term abdominal pain, diarrhea, weight loss, or anemia.
The diagnostic process typically begins with blood tests. A complete blood count can reveal anemia, increased white blood cells, or elevated platelets, all of which may indicate inflammation. Additional tests, such as the erythrocyte sedimentation rate and the C-reactive protein test, can also detect signs of inflammation. Some children may have low levels of albumin, a protein made by the liver, which can occur when inflammation is present. While these tests can suggest Crohn’s disease, they are not enough to confirm the diagnosis on their own, as other conditions can cause similar results.
A stool sample is often collected to rule out infections or parasites that could cause similar symptoms. Stool testing can also detect hidden blood and measure fecal calprotectin, a protein that signals inflammation in the intestines and helps doctors distinguish inflammatory bowel disease from other digestive problems.
Imaging studies are another important part of diagnosis. X-rays, CT scans, and MRI scans can help visualize the intestines and identify areas of inflammation, narrowing, or other abnormalities. More specialized imaging tests, such as magnetic resonance enterography (MRE) and computed tomography enterography (CTE), use contrast liquid to create detailed images of the small intestine and show inflammation or bleeding. Some centers also use ultrasound to safely and noninvasively view the digestive organs.
Direct visual examinations of the digestive tract are key diagnostic tools. An upper endoscopy allows doctors to view the esophagus, stomach, and the first section of the small intestine by inserting a flexible tube with a camera through the mouth. This test helps detect visible inflammation and allows for tissue biopsies to confirm microscopic disease. A colonoscopy examines the rectum, colon, and the last part of the small intestine through the anus and also allows biopsy samples to be taken.
Another advanced test is video capsule endoscopy, which has been approved for use in children over the age of two. In this procedure, the child swallows a small capsule containing a miniature camera that takes thousands of pictures as it moves through the digestive tract. The images are transmitted to a recorder worn by the patient. This test allows doctors to see parts of the small intestine that cannot be reached with traditional endoscopy or colonoscopy, although it does not allow tissue samples to be taken.
Treatment:
Treating pediatric Crohn’s disease often requires a team of specialists working together to create a personalized care plan. This team may include pediatricians, gastroenterologists, surgeons, psychologists, dietitians, nutritionists, and other healthcare professionals. Because the disease affects both physical and emotional well-being, psychosocial support for the child and family is an important part of care. Although there is no cure for Crohn’s disease, proper treatment and support can help manage symptoms, achieve remission, and allow children to live healthy, active lives.
Treatment plans vary depending on the child’s symptoms and disease severity. What works well for one child may not be as effective for another, so decisions about medications or other treatments are made carefully between the healthcare team, the child, and the parents. The main goals of therapy are to reduce inflammation, relieve symptoms, improve growth and nutrition, and maintain remission to prevent complications. Treatment usually involves a combination of medications, dietary management, and sometimes surgery.
For children with mild or moderate disease, doctors may prescribe 5-aminosalicylic acid (5-ASA), a medication that helps control inflammation. Those with more severe disease may need corticosteroids, which are stronger anti-inflammatory drugs that can bring active disease under control and help achieve remission. Antibiotics may also be used to treat intestinal bacteria that can worsen inflammation or cause infections related to perianal disease, abscesses, or fistulas. Immunomodulators, such as 6-mercaptopurine, azathioprine, and methotrexate, help regulate the immune system and can be used to maintain remission.
Nutritional therapy plays an important role in treatment. While there is no single diet proven to cure Crohn’s disease, doctors often recommend avoiding foods that are hard to digest, such as raw vegetables, nuts, or popcorn, especially when parts of the bowel are narrowed. Some foods, like milk or spicy dishes, may worsen symptoms for certain children. Because inflammation can interfere with nutrient absorption, children may struggle to grow or gain weight. In some cases, exclusive enteral nutrition (EEN) is prescribed, where all calories come from a special liquid formula instead of regular food. This formula can be taken by mouth or delivered directly into the stomach through a thin tube inserted through the nose. EEN not only improves nutrition but can also help bring active disease into remission.
Surgery is considered when medications and diet changes do not adequately control the disease. The most common procedure involves removing diseased portions of the intestines, although Crohn’s disease can return in nearby areas. About half of children who have surgery will eventually need another operation. In more severe cases, removing larger sections of the intestine may lead to short bowel syndrome, a condition where the remaining intestine cannot absorb enough nutrients. Surgery may also be required for intestinal blockages, severe bleeding, fistulas, perforations, or abscesses that do not respond to other treatments.
How You Can Make an Impact:
Without proper research, funding, and support for continued studies and clinical trials to determine possible cures, legitimate medicines for the disease, or preventative treatment, many more children will go on to develop Crohn’s Disease. If you can, please donate here! If you are unable to donate, consider volunteering your time by raising awareness for this rare disease. If you’re interested in learning more about Crohn’s Disease, donation opportunities, or the progress being made on potential treatments, visit the Pediatric IBD Foundation. The Pediatric IBD Foundation strives to “improve the lives of children with Crohn’s disease and ulcerative colitis through advocacy and education.”
References:
Stein, R. E. (2023, August 4). Pediatric Crohn’s Disease – Symptoms, Causes, Treatment | NORD. NORD (National Organization for Rare Disorders); NORD. https://rarediseases.org/rare-diseases/pediatric-crohns-disease/
Leave a comment